May 28, 2019
This past week’s interest has been on frozen shoulder due to meeting one of Teresa’s patients who presented with this condition and discussing some of the questions they had. Frozen shoulder, or less commonly known as adhesive capsulitis, is a self-limiting condition that results in shoulder pain and large mobility deficits. However, it’s a disease that still has a lot of question marks as to why it happens, who it happens to, and how to speed up the recovery process.
Therefore, I’ve taken this opportunity to do some research myself, to see if there are any current findings that can help answer any of these questions. An article that I came across by Filip Struyf and Mira Meeus (2014) focused on the effects of physiotherapy in someone with frozen shoulder. The purpose of this article was to provide new insights in physiotherapists policy in treating frozen shoulder.
What Is Frozen Shoulder?
Adhesive capsulitis, or frozen shoulder, defined by this article is the loss of range of motion (ROM) greater than 25% in at least two movement planes, combined with at least 50% loss of passive external rotation in comparison to the unaffected shoulder. Considering the shoulder joints unique capsule pattern, someone presenting with frozen shoulder will have limitations in external rotation more than abduction which is more limited than internal rotation.
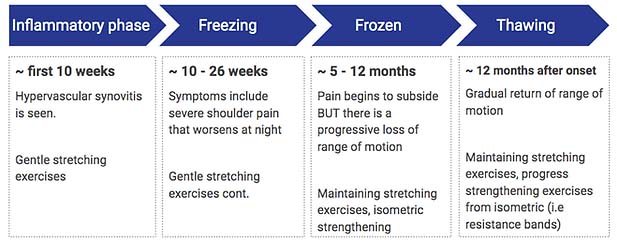
Another important factor to note about frozen shoulder is that it progresses through a continuum of phases that present with different symptoms and should be treated accordingly:
Inflammatory phase: The shoulder joint capsule ligaments become inflamed, as cytokines and other inflammatory molecules are released and trigger the local nociceptors.
Freezing: In this phase inflammation is increasing, causing the pain to worsen and diffuse through the shoulder.
Frozen: Over time, active shoulder inflammation decreases as local connective tissue scarring increases. The accumulation of scar tissue in the joint capsule results in a decrease in the volume of space which in turn causes shoulder stiffness and progressive restriction of shoulder movement.
Thawing: In this phase, scar tissue in the joint capsule eventually begins to break down by itself, to be replaced by healthy, flexible ligaments. Joint space and joint capsule mobility are gradually restored.
Physiotherapy, Can It Help?
Filip and Meeus (2014) have suggested that indeed, physiotherapy is beneficial in alleviating pain, improving functionality, and regaining ROM. It has been proven to be especially important in the later phases of the disease because stretching of the joint capsule helps to break down scar tissue faster, which can speed up recovery time and help prevent the total loss of ROM.

However, if the physiotherapy regime is too aggressive, it can cause more inflammation in the joint which may worsen the symptoms. Considering this, Filip and Meeus (2014) have suggested that principles for treating patients with frozen shoulder should be determined by the tissues ability to cope with physical stress or “tissue irritability”. This subjective approach will help determine whether a specific therapeutic modality is appropriate at that time, what kind of intensity to apply, and how long to how often to perform these treatments.
The notion of frozen shoulder recovery being a gradual process, gave me the idea that perhaps we need to approach treatment of this condition similar to the way concussions are treated. A concussion is treated in small steps, based on the presence and severity of symptoms. In fact, a study performed by Kelly, McClure and Leggin (2009) treated patients with frozen shoulder based on their score of tissue irritability using a visual analog scale. They found that this process was successful in reducing pain as well as made the recovery process more manageable for patients suffering through the course of the disease.
All considered, frozen shoulder is a very frustrating disease to cope with, and unfortunately a lot of research gaps remain. However, it’s proven physiotherapy can make a positive difference with appropriate treatment. Most importantly, while providing treatment, one should be conscious of their patient’s mental state and promote activity modifications to encourage functional, pain-free range of motion.